Using patient data across the world
Patients are voluntarily making their data and specimens freely available to researchers. But the biobanks still have some legal gaps to bridge.

The container with the frozen samples of blood and other bodily fluids is scanned before its automatic dispatch into the -150° C tank. | Image: InselGruppe/Pascal Gugler
On the last day of the 2017 spring session of parliament, the Socialist Party’s National Councillor Rebecca Ruiz from the canton of Vaud proposed a motion to create a biobank law.
“Biobanks in which data and specimens from patient treatments are collected and evaluated are rapidly increasing in importance”, says Ruiz. “But current laws are deficient in their coverage of them”. Her proposal received the support of 23 members of parliament.
The occasion came at the end of March with the conclusion of the consultation process for the ‘general consent’ that has been devised jointly by the Swiss Academy of Medical Sciences and Swissethics. If hospital patients sign this form, their data and specimens can be utilised in future, as yet undefined research projects. University hospitals have already been working with such general consent forms for a while now, though they still differ from one canton to another. The proposed general consent would be the first time that there has been a single, standardised, national form.
Lack of data security in hospitals
But a source of delight for scientists is a cause for concern for patient protection organisations. Franziska Sprecher is a professor of law in Bern who represents the patient protection organisation SPO, and she is critical of the current state of affairs. “It’s not acceptable that there is only a patchy legal basis for something as important as biomedical research and handling patient specimens and digitised data”. Hospitals are too lax in providing data security, she says, and if there is a data breach, then the patients will be left pretty much to cope on their own.
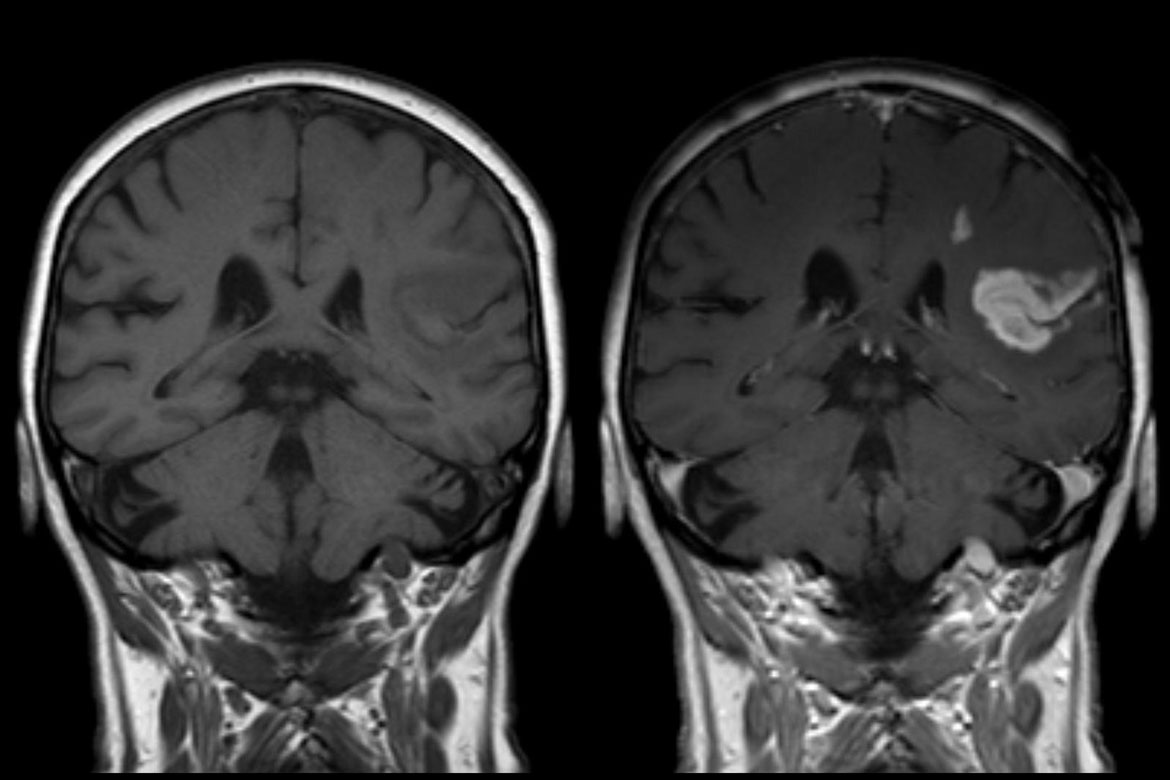
So why is general consent so important for biomedical research? Vincent Mooser is a laboratory pathologist who has been running a pioneering biobank with blood specimens at the Lausanne University Hospital (CHUV) since 2013. He explains it as follows: “In order to be successful in the field of personalised medicine, we need data from very, very many people”. As an example, Mooser mentions the CoLaus Study, which began in Lausanne in 2003 with the goal of identifying cardiovascular-disease risk factors. The Lausanne group has over 6,000 patients and is a success, but in order to get further results, CHUV will have to cooperate with other hospitals.
Research on a very different scale
With a general consent form, it will become possible to exchange data, both within Switzerland and with foreign laboratories. “We will be doing research on a very different scale altogether”, says Mooser. This is essential in order to remain internationally competitive. Other countries, like the USA, the United Kingdom, China and India have long begun using big data in their medical research. Besides, he says, general consent does not offer up a blank cheque: “Researchers need the permission of their ethics commission for every project they undertake”.
In fact, Swiss citizens aren’t reticent about sharing their health data for research purposes. At CHUV, for example, three out of four patients agree to donate their data, even if it goes so far as analysing their whole genome. At the University Hospital in Basel, the percentage is even higher. Up to today, over 27,000 general consent forms have been signed in Lausanne. For Mooser, it is natural that their corresponding data and specimens are protected to the highest possible security standards.
CHUV is also home to the offices of the Swiss Biobanking Platform, and the big Swiss biobanks have joined it. On their website, they state that they welcome Ruiz’s motion to create a biobank law. For the time being, the network has accepted the rules of the Declaration of Taipei, issued by the World Medical Association in 2016, which lays down fundamental guidelines for running biobanks. Sprecher sees this as sending out a “strong signal”, but she still wants more to happen. She believes that the Declaration has to become part of the professional ethics guidelines for doctors.
Irène Dietschi is a freelance science journalist in Olten.